Nutritional support and Healthy Lifestyle choices can aid your recovery
With more than 65 million reported cases of COVID-19 in the U.S. alone (and rising), many people are experiencing symptoms for weeks and even months after the infection has cleared. Recovering from COVID does not guarantee that everyone will return to their usual state of health. You may wonder why some viruses leave lasting effects on us, zapping our energy and impacting our ability to thrive.
What are the Symptoms of Long-Haul Covid and Who’s Impacted?
The answer is not clear yet, but here’s what we know: If you or a loved one contracted COVID and are now suffering with a lingering list of symptoms, you may be suffering from post-acute sequelae, or consequences, of SARS CoV2 (PASC), also known as “Long COVID” or Long Haulers Syndrome (LHS). Symptoms can include fatigue, shortness of breath, cognitive dysfunction, neurological issues, persistent headache, rashes, gut-related disturbances, and lasting changes to your sense of taste and smell.
Tens of thousands of people in the U.S. have lingering illness following COVID. It is reported that 50-80% of patients continue to experience bothersome symptoms three months after the onset of the acute infection, long after tests no longer detect the virus in their system. Studies show that 15-33% of COVID patients develop long-haul symptoms, and European studies quote significantly higher statistics.
It is believed that risk factors such as obesity and Type 2 diabetes can increase the risk of developing more severe symptoms of COVID, but this is not necessarily true for LHS. Surprisingly, the data shows that hospitalized COVID patients did not have a higher incidence of developing LHS. Furthermore, the data indicates that those with less severe cases of COVID were at equal risk of developing LHS as those who required hospitalization. While the long-term prognosis for full recovery is uncertain, the medical profession remains hopeful for a better understanding.
Theories About Long Haulers Syndrome Causes
Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, has speculated that LHS is similar to post viral myalgic encephalomyelitis/chronic fatigue syndrome. This can be triggered by Mononucleosis, Lyme, or other SARS infections. One possible explanation for LHS is a persistent state of chronic low-grade inflammation in the brain or spinal cord, generated by the disease or possibly by a faulty host immune response to the virus.
, Professor Akiko Iwasaki has a different theory. He calls LHS a viral ghost, because fragments of the virus can linger after the infection is cleared, causing persistent activation of the immune system. This overstimulation leads to “the cell danger response,” triggered when we encounter a threat that exceeds our cellular capacity for homeostasis. Because the immune system uses over 50% of our daily supply of energy when it ramps out of control, we can run out of energy quickly. This response can also trigger the reactivation of other viruses like Epstein Barr. This is similar to chronic inflammatory response syndrome (CIRS) seen with mold and Lyme disease.
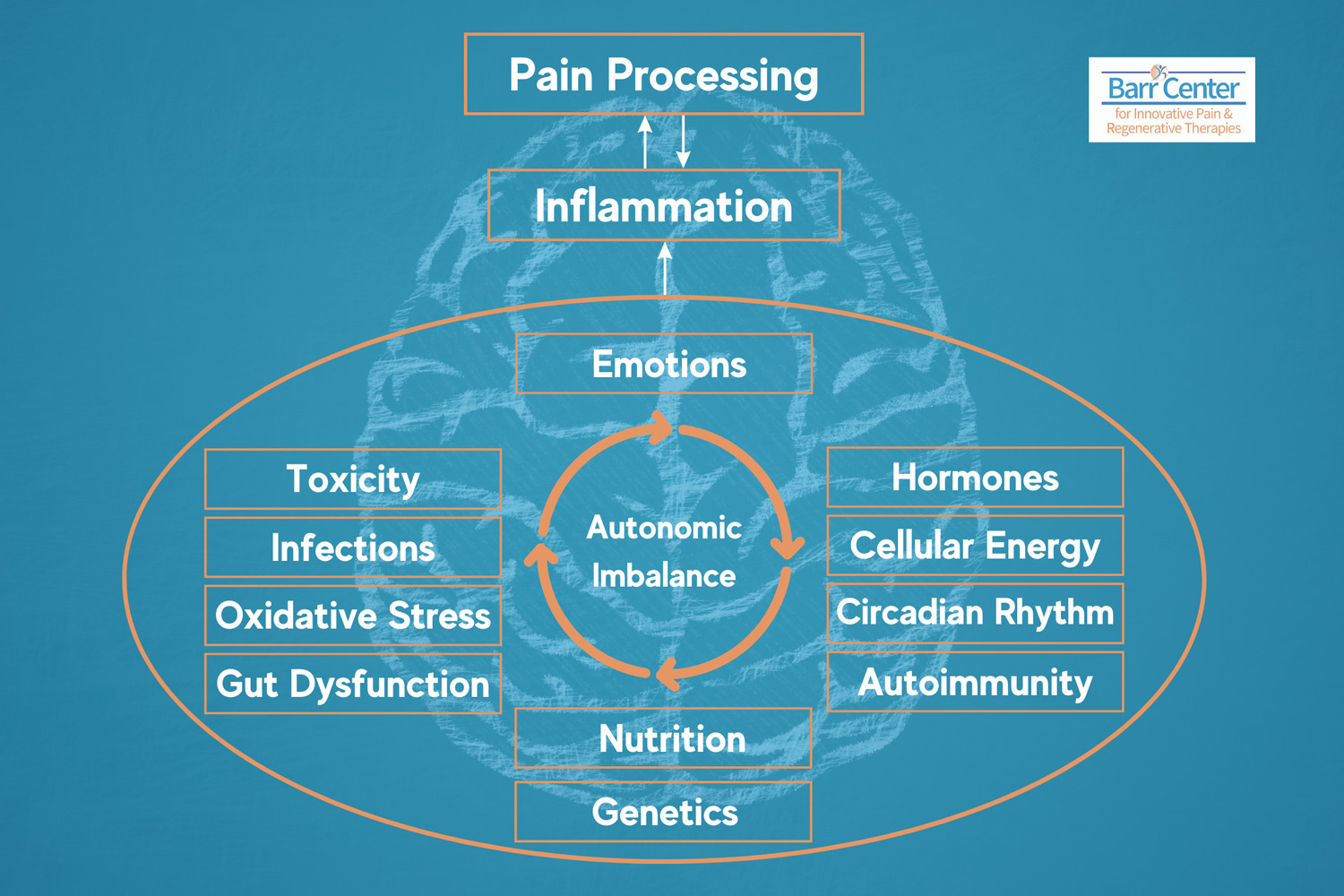
The truth is we are just beginning to understand the underlying causes of LHS symptoms. Some are caused by direct damage to organs, such as the lungs, and others are due to persistent inflammation and immune activation. Still other symptoms are caused by deeper damage at the cellular level, affecting the mitochondria and ACE2 enzyme activity.
The Role of Mitochondria in Long Haul COVID Treatment
Mitochondrial dysfunction may also play a role in COVID recovery. Mitochondria produce energy for all cells; it is concentrated highest in the brain (nervous system) and heart (muscle). Because our immune system requires a lot of our daily energy production, mitochondrial function is the key to staying healthy and recovering from infections.
Additionally, free radical damage (or oxidative stress) caused by a significant viral infection can harm our mitochondria. This may contribute to many of the symptoms that people experience, especially fatigue, brain fog and cognitive impairment.
Therefore, to treat Long Haul COVID from a functional medicine perspective, we need to work on restoring and improving the function of the mitochondria, in addition to reducing inflammation and rebalancing the immune system.
Healthy lifestyle changes can help your mitochondria recover and combat free radicals. Here are some helpful tips to optimize mitochondrial function:
- Eat a diet rich in plants, especially antioxidants. This is key! Antioxidants are found in Vitamin A, Beta-carotene, Vitamins C and E and polyphenols found in the rich colors of a rainbow diet—fruits and veggies that are red, orange, yellow, green, and purple. Additionally, mitochondria love a compound called PQQ. Eating PQQ-rich foods is a great idea. These include parsley, green peppers, kiwi fruit, papaya, green tea, and tofu. The Barr Center’s Mitocell PQQ is a great supplement option to support your mitochondria.
- Exercise, with a focus on high-intensity interval training (HIIT) and reconditioning helps build muscle and activates stem cell production. Also, it’s important to know that excessive strenuous exercise can cause unwanted oxidative stress and cause you to “crash” the next day. The best way to slowly regain your stamina is to exercise at a level that you can sustain, day after day without “crashing.”
- Get a good night’s sleep. When we sleep effectively, we move into the “rest-and-digest” mode. This parasympathetic state is necessary for healing. Critical repair happens at night, so aim to sleep for at least 7- 8 hours each night. If you have difficulty falling or staying asleep, you may benefit from supplements, medication and lifestyle changes that help promote healthy sleep hygiene. . Wearing a Fitbit, Apple Watch or Oura ring can help you track your sleep, to see how changes translate into improved sleep quality and improved resilience.
- Try intravenous vitamin therapy. In conjunction with the right diet, proper sleep and easing into exercise, Intravenous Vitamin Therapy can also benefit COVID recovery. Hang 10 Drips offers an IVinfusion protocol, the Longboard, to help recover from COVID. As a partner in this new venture, I developed this drip protocol. It uses intravenous vitamins, powerful antioxidants and amino acids that work deep within the cells, to help with the recovery and repair of damage done to the mitochondria. It can help reduce inflammation and give your immune system and cells a reboot after fighting to clear a COVID-19 infection.With so many people experiencing gut issues after a COVID infection, we believe the best way to receive these nutrients is through an IV. An IV infusion bypasses the GI tract, ensuring your cells absorb 100% of our targeted formulation to help you recover and feel like your old self.
In summary, while this virus and its after-effects are changing life as we know it, the most important thing we can do is to manage stress effectively and support our immune systems as much as possible. This means getting good nutrition, adequate hydration, a good night’s sleep and monitoring our gut health. When you need that extra boost of nutrients, mitochondrial and immune support following Covid, or other infections come in and experience the Longboard protocol. See for yourself how effective our specialized IV nutrition protocol can be at helping to get your health back on track.
Scheduling Appointment for IV Therapy
To schedule an appointment with the Barr Center or Hang 10 Drips, contact us at 757-578-2260 or schedule an appointment online.
_____________
*The Longboard protocol includes three infusions. The first part is a foundational immune-boosting drip with added L-Carnitine (note: thyroid precautions) and NAC. The second part is Alpha Lipoic Acid and the third Glutathione. COQ10, additional Vitamin C and IM injections of Vitamin D are also available.