Many of our patients ask, “What is the Best Treatment for Arthritis in Lower Back?” Pain, stiffness, and soft tissue tightness are common symptoms of arthritis of the spine. Some people even feel painful soft tissue nodules over their inflamed joints.
Arthritis of the neck and back impacts people’s quality of life, affecting 85% of people over the age of 60. While wear and tear takes its toll as we age, even young people experience pain from arthritis in these areas. Typically, in younger people, arthritis of the back and neck is due to trauma, sports injuries or overuse.
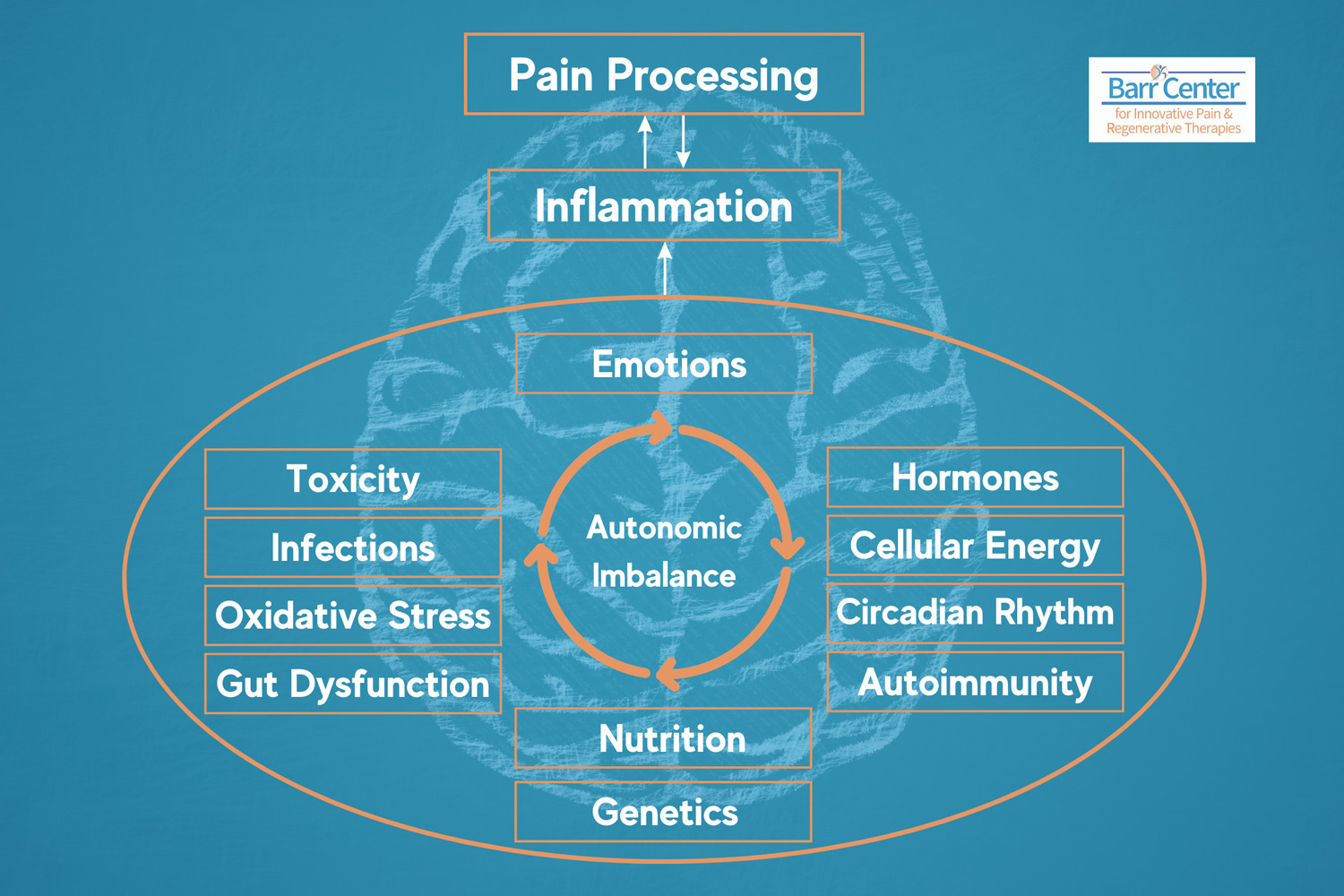
People at any age can experience pain due to facet joint inflammation if they have gut-mediated inflammation stemming from inflammatory bowel disorders, leaky gut, food sensitivities or IBS. The most common food sensitivities being gluten and dairy. Not sure if this is your issue? Functional Medicine testing can help us identify if this is a potential concern and help uncover other hidden sources of pain.
Now the good news – regardless of the cause, you don’t have to suffer with these symptoms. There are effective non-surgical treatments to reduce and/or eliminate symptoms of arthritis of the back and neck. Before we get to the treatment options, let’s briefly explain the anatomy of the spine.
Lower Spine Pain Explained
Our spine has two columns of support; in the front are the discs and vertebral bodies, and in the back are paired facet (“hinge”) joints that open and close when we move. Bending forward opens the facets, and bending backward closes them. Rotation torques them.
Each facet joint has a capsule that contains joint fluid keeping it healthy. Inflammation can cause a buildup of inflammatory synovial fluid in these joints making pain symptoms worse. Additional supporting structures include muscles, tendons and ligaments and fascia, and they can be affected as well.
The facet joints have a seesaw relationship with the discs. If you have disc degeneration, the corresponding facet joints will degenerate. This process is called spondylosis. Interestingly, not all joints in a spine with spondylosis cause pain; usually, it’s those inflamed or unstable joints that hurt.
All facet joints have well-defined pain referral patterns. This is particularly true in the neck. This is why it is important to closely correlate your degenerative changes with your unique pain pattern. If your pain pattern fits the findings on your x-rays, CT or MRI imaging, then it is important to block the affected joints with a local anesthetic and see if the pain goes away.
What is the Best Treatment for Arthritis in Lower Back?
The process of blocking the joints is minimally invasive and is called diagnostic Medial Branch Blocks (DMBBs). DMBBs are diagnostic but not therapeutic. They are a necessary step in defining and confirming the pain generator.
DMBBs are performed safely in our procedure room using x-ray guidance, a small needle, x-ray contrast and both a long and short-acting local anesthetic. The procedure is not very painful and is low risk-taking 15-30 minutes.
The relief is designed to provide you with about an 8-hour testing window. You will be sent home with a post to document how successful we were in blocking your pain. This will help us identify if the injected facet joints are actually your pain generator. This completed pain diary ultimately becomes part of your chart and helps to guide treatment.
Once we identify and then confirm which facet joints are your pain generator, then we can move forward with definitive treatment. This means that if you respond positively to the medial branch blocks, then we will have to repeat them and document a reproducible response. Once this is all documented at your follow-up visits, we can seek authorization from your insurance company to get coverage for the definitive procedure called radiofrequency ablation (RFA).
While a permanent cure for osteoarthritis of the spine does not exist, it can be helped with medial branch blocks and radiofrequency ablation. It should be noted that most insurance companies only cover DMBBs leading to radiofrequency ablation.
In the past, we often performed actual facet joint injections using steroids and lidocaine but now this treatment approach has been replaced by the above DMBBs leading to RFA. Some exceptions to this policy include a pacemaker, a facet cyst, instability of the spine or a prior fusion surgery. If these conditions exist, then we will seek special authorization for the facet joint injections with steroids but here is no guarantee that it will be authorized.
How Facet Join Injections Help Lower Back and Neck Pain
Facet joint injections with steroids reduces inflammation in the affected joints as opposed to RFA which works by cauterizing the nerve that supplies sensation to the facet joint. While the treatment goals are the same, the pain-relieving methods are quite different. RFA destroys these small nerves for periods of time ranging from 6-24 months, while the steroid reduces swelling, inflammation, and pain in the joint for an unspecified period- usually months.
Because the studies performed to date reveal a longer period of relief from the RFA, most insurance companies are no longer covering the steroid-based facet joint injections. This certainly does not mean that they are in no way less effective.
Treatment coverage decisions are based on what the medical literature says is “evidence based” and is not based on past performance. This change has been frustrating to our established patients who are used to benefitting from steroid-based facet joint injections.
As an alternative, PRP (platelet rich plasma) or bone marrow-derived stem cell injections can be performed into the facet joints in lieu of steroids and can yield long lasting relief of pain due to inflammation and degeneration. These regenerative procedures are not covered by insurance and are self-pay.
Regenerative Medicine and Prolotherapy
Another regenerative therapy, Prolotherapy, deserves a mention as a beneficial therapy for arthritis of the back and neck especially when there is evidence of hypermobility or ligament laxity due to ligament strain, overuse, whiplash etc. Prolotherapy is a procedure similar to the facet joint injections and PRP but instead of injecting steroid or PRP the joints and surrounding ligaments are injected with an irritant solution consisting of hypertonic dextrose, phenol, glycerin and Lidocaine in a mixture designed to cause localized inflammation.
The ultimate goal of prolotherapy is to tighten ligaments and surrounding joint capsules, making the spine more stable. This procedure is a wonderful way to manage chronic back and neck pain but is also not covered by any insurance plan. It is something that we have a great deal of experience with and detailed information about prolotherapy and PRP is available on our website www.BarrCenter.com.
Frequently Asked Questions (FAQS)
1. WHAT IS RADIOFREQUENCY ABLATION?
Radiofrequency ablation (RFA) stops pain signals from reaching the brain by burning the nerve endings responsible for your pain. RFA uses radiofrequency waves, similar to microwaves, to heat up the targeted nerves and render them unable to conduct pain signals. It is in a fashion like disabling an alarm system- once those nerve endings no longer exist, they can no longer send pain signals to your brain. The arthritis is still there, but you can’t feel it.
2. WHAT IF I AM ON A BLOOD THINNER?
We have different size needles that produce different size lesions. If you bleed easily or are on a blood thinner, then we use a smaller needle. Please note the advantage of using the larger needles is that the duration of the relief is longer as the lesion is larger. If you are not sure which to choose, ask our staff to discuss these options with you further.
3. WHAT IF I HAVE AN ALLERGY TO X-RAY CONTRAST?
We do use a small amount of x-ray contrast for DMBBs but not RFA, and thus if you have a contrast allergy, you will need to take the Radin prep beforehand, and this will need to be prescribed in advance of the day of the procedure. In the case of severe allergy, we may opt to perform the procedure without contrast.
4. DOES RFA PERMANENTLY DAMAGE THE NERVES?
The main advantage of RFA treatments is that they typically last for a long time. Yes, your nerve endings eventually grow back, but they regenerate quite slowly. Thus, pain relief from RFA lasts for a year or more on average; however, regeneration time varies from patient to patient.
What You Should Know Before Your Procedure:
- Please come to your procedure appointment well-hydrated. Drinking more water than usual is best. This applies to all procedures.
- Please arrange to have a driver drive you home after any of these procedures as it is not safe to drive for 4-8 hours, depending on which procedure you have.
- Please inform our staff of any history of contrast allergy several days prior to your scheduled procedure.
- If you are undergoing PRP, Stem cell or Prolotherapy injections, please avoid the use of NSAIDs like Motrin or Aleve prior to and following your injections.
- If you have a pacemaker, you are NOT a candidate for RFA. Please let us know if you have had a pacemaker placed since your last visit.
What Can You Expect After Your Procedure:
- You will likely experience transient numbness after all facet-related procedures. This is from the local anesthetic, and the numbness can last between 4-8 hours. You can also feel somewhat dizzy after the cervical procedures. It is for this reason that we require you to have a driver.
- Post-procedure soreness is more common with the RFA and can last from 7-30 days.
- If you notice redness or swelling in the injection sites or develop a fever, please notify us ASAP.
- Ice packs and Lidocaine patches can come in handy to manage post-injection swelling and/or soreness.
- If appropriate, Tylenol, Motrin and other mild pain relievers can be helpful with post-procedural pain. If you anticipate needing a refill on one of your medications, please let us know when you come back to have your vitals checked prior to the procedure. Occasionally, we will provide you with a 1-week prescription of a mild pain reliever after your procedure. Continued use of opioids is discouraged.
What is the Best Treatment for Arthritis in Lower Back? Schedule a Consultation to Learn About Your Options.
It’s easy to see how each treatment approach has different advantages and disadvantages. Plus, each treatment modality doesn’t have to be an “either-or.” if you’re living with arthritis or experiencing neck or back stiffness and pain, it might be time to speak to one of our Barr Center clinicians to determine the root cause of your pain.
Call the Barr Center for Innovative Pain & Regenerative Therapies today for a consultation, review of your condition and best treatment options at 757-578-2260.
Copyright 2022 Barr Center