Intervertebral Discs – Herniated Disc or Sciatica
What are the intervertebral discs and how do discs degenerate?
They is a circular ligament called the annulus fibrosus surrounding a gel-like system called the nucleus pulposus that functions as a shock absorber between the vertebrae. The discs make up about one-fourth of the height of the spinal column. They serve as spacers and cushions for the spine and allow for spinal mobility. The center of the disc, called the nucleus pulposus, is surrounded by the annulus fibrosus which is semi-gelatinous and fluid-like, composed mainly of protein aggregates and water. At birth, the water content of a disc is about 90 percent, but it gradually decreases with age. By the time we are in our fifties, the water content can decrease to 70 percent or more. This is what leads to age related disc degeneration and explains why we shrink in height as we age. The term “degenerative disc disease” is really a misnomer. The degeneration of the disc is a natural process of aging and overuse, resulting in deterioration. The term “disease” is also a misnomer as it is not a disease, but a process. It is frequently referred to as “DDD”. As the discs shrink in height the connecting joints of the spine called facet joints enlarge. This condition is called spondylosis.
Age, genetics and environmental factors result in changes within the discs. Blood supply to the discs decreases and the discs gradually deteriorate and lose water. When this process progresses the differentiation between the outer ligamentous annulus and the inner gel-like nucleus becomes less distinguishable. This deterioration results in:
- Decreased spinal range of motion
- Decreased ability for the disc to function as a shock absorber for the spine
- Decreased vertebral column height
- Increased weight-bearing and possible irritation and enlargement of the facet joints
- Risk of increased compression of the spinal nerves
- Risk of development of pain as a result of the changes in the disc
Herniated Disc
What is a Herniated Disc?
The fissures in the outer fibers (annulus pulposus) may become extensive, and the nucleus pulposus (the center of the disc) may start to squeeze through to the edge of the disc or beyond. This will cause the disc to bulge initially, and when the deterioration occurs through most or all of the layers, a true herniation will result. The herniation will be defined as a bulge protrusion or extrusion, depending upon the shape of the herniation.
Disc protrusions may compress spinal nerves or the spinal cord, which can result in leg pain or sciatica. Herniated discs are also referred to as “slipped” disc. A herniated disc can occur in any part of your spine, but it tends to occur more frequently in the lumbar spine (low back) than the cervical spine (neck) and less frequently in the thoracic spine (mid back). When the nuclear material of the disc protrudes completely through the annulus and is effectively a ‘free fragment’ we call this a disc extrusion.
Sciatica
What is Sciatica?
 When you experience low back pain and/or leg pain that radiates from the buttock as far down as the foot, the culprit may well be sciatica.
When you experience low back pain and/or leg pain that radiates from the buttock as far down as the foot, the culprit may well be sciatica.
The problem may result from irritation to the sciatic nerve (a large nerve that runs from the low back down the leg). It can be caused by compression of one of the nerve roots that make up the sciatic nerve. It can also be caused by compression of the sciatic nerve itself, which is less common. Piriformis syndrome and rare tumors of the sciatic nerve can cause pain to radiate down the leg. The sciatic nerve provides partial sensation and motor control to the leg, and when it is compromised by pain, numbness and weakness could result. The nerves that make up the sciatic nerve exit the spine at each level on each side. These are called segmental nerves and The sciatic nerve is made up of branches of L4- S4. Each nerve is laminated like the rings of a tree with the outer fibers being the sensory fibers and the inner fibers that are more insulated being the motor fibers.
Pain from a herniated disc can start in the low back, then progressively go down the leg, and usually will only affect one side of your body
Pain from a disc problem can mimic other medical problems, particularly muscular problems such as piriformis syndrome.
An accurate diagnosis is made as a result of a thorough history and physical evaluation as well as other diagnostic testing, which may include:
- MRI
- Electromyography/Nerve Conduction Velocity Test (EMG/NCV)
- CT Scan
- Provocation Discography
- Myelogram
- Diagnostic spinal injection
How is it treated?
Symptoms from a herniated disc usually improve in a few weeks or months. To help you recover:
- Stay active (walk or do other light activity).
- Rest if you have severe pain.
- For an acute injury, apply ice for 10-15 minutes, three times per day, for two to three days. After three days you can start to use heat help further reduce the pain.
- Take medication to relieve pain. Medication will not cure a disc herniation.
- Undergo physical therapy, for instruction in doing exercises properly.
- Spinal injections may be recommended in certain cases.
- Surgery may be recommended for cases that do not respond to conservative treatment.
Treatments for lumbar disc herniations and Spinal Stenosis includes:
Epidural Steroid Injections and Selective Nerve Root Blocks
What are epidural steroid injections?
An epidural steroid injection is a spinal procedure in which a steroid and usually an anesthetic are injected in the spinal region called the epidural space. The nerves, spinal fluid, and spinal cord are enclosed within a membrane sack called the dura. The injection is outside this membrane. It is useful to reduce inflammation from nerve roots or intervertebral discs. Decreasing the inflammation may decrease the pain originating from these structures.
What are the different types of epidural steroid injections?
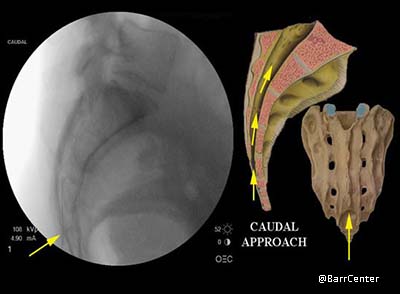
Caudal: the injection is placed through a small opening (sacral canal) just above the tailbone.
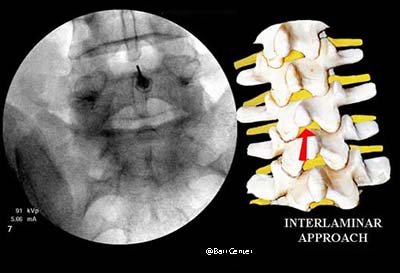
Interlaminar: the injection is usually midline and placed directly between two vertebrae (similar to the approach a woman undergoes during labor for epidural anesthesia).
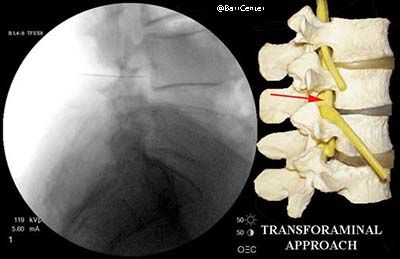
Transforaminal: the injection is placed in the foramina (opening) on the side of the spine near the exiting nerve. This is often the preferred method of injection as the needle and cortisone gets very close to the offending disc herniation yielding quick relief and often very good results.
Selective Nerve Root Blocks
What are selective nerve root blocks?
A selective nerve root block is a spinal procedure in which anesthetic is placed on a specific nerve root of the spine to help identify the exact source of leg pain. This can be used as a purely diagnostic test when we need to determine the best level for injection and surgical intervention. The injection usually also contains steroid to decrease inflammation and pain. The injection is similar to a transforaminal epidural steroid injection, but in a selective nerve root block there is no attempt to have the medication enter the epidural space. Rather, the aim is strictly to cover the offending nerve root.
How are selective nerve root blocks and epidural steroid injections performed?
The procedure is usually done with the patient lying on his or her stomach under fluoroscopic X-ray.
The skin is cleaned thoroughly with antiseptic solution before the injection is performed. After the skin has been numbed with local anesthetic, a small spinal needle is inserted under fluoroscopic guidance to the appropriate position within the spine.
For selective nerve root blocks and the transforaminal approach for an epidural steroid injection, the final needle position is just above the target nerve root.
In the caudal approach for an epidural steroid injection, the needle is passed through a small opening (sacral canal) just above the tailbone.
With the interlaminar approach of an epidural steroid injection, the needle is passed between two vertebrae, usually midline. Contrast dye is injected to confirm proper needle position.
The medication is then injected. The patient’s vital signs are closely monitored during the procedure, which takes about 15 to 30 minutes. After the injection, the patient is taken to the post-procedure area for continued monitoring.
What is actually injected?
The injection usually consists of a mixture of a local anesthetic (e.g., Marcaine®, Lidocaine) and the steroid injection (e.g., Dexamethasone or Celestone).
Is the procedure painful?
Not usually. Most patients say it is about as painful as a routine blood test.
What should I expect after the procedure?
If anesthetic is placed around a nerve root or epidural space, you may experience a period of numbness in that region or limb for 3 to 8 hours. The steroid medication may begin working anywhere from 6 hours to 3 days after the injection. Some individuals do experience a period of soreness 1 to 2 days after the injection. An application of ice may help during this period. Within one to five days, you may start noticing significant pain relief.
What should I do after the procedure?
After the procedure, you should have someone drive you home. It is advised that patients minimize their activity and take it easy for a day or so after the procedure. If there is soreness at the injection site, you can apply ice to the area.
How soon can I return to work?
The day after the procedure, you can perform normal activities as long as they are not uncomfortable.
How many injections should I have?
We generally do not perform more than three injections within a 12-month period. Very frequent injections may increase the likelihood of side effects from the steroid.
Are there any risks with this procedure?
This is considered a very safe procedure. However, as with any procedure, there are risks and possible side effects or complications.
The complications from the selective nerve root blocks and epidural steroid injection include:
- Pain at the injection site – common
- Worsening of symptoms – occasional
- Infection – rare
- Bleeding – rare
- Serious nerve or spinal cord injury – extremely rare
Other side effects are generally related to the steroid medication and may include:
- Fluid retention – uncommon
- Weight gain – uncommon
- Elevated blood pressure – uncommon
- Mood swings – rare
- Insomnia – rare
- Suppression of the body’s own natural production of cortisone – rare
Can I have this procedure if I am on Coumadin® or other blood thinners?
No. You should not have the procedure if you are currently taking blood-thinning medication such as Coumadin® or Plavix®. You may be asked to temporarily stop your blood-thinning medication, but do not do so without discussing this with your doctor.
Who should not receive a selective nerve root block or epidural steroid injection?
You should not undergo a selective nerve root block or epidural steroid injection if:
- You are prone to excessive bleeding or you are taking anticoagulant (blood thinning) medication.
- Your back pain has been diagnosed as being the result of an infection or malignancy.
- There is any systemic bacterial infection or local skin infection near the injection site.
Can the Barr Center Help You with Back Pain Relief?
Call us at 757-578-2260 or email us at [email protected] to get started on relieving your back pain.
Learn More
Other pain management conditions we treat are: Neck Pain, Shoulder Pain, Hip Pain and Knee Pain. We often use Regenerative Medicine and Physical Therapy in our treatments.










