This blog post is personal. I feel compelled to share my story about pain and oxalates. Like many during the first year of Covid, my diet and activity level changed dramatically. Considerable Covid stress plus the uncertainties of opening a new medical practice during those crazy times threw my regular routine into a tailspin. Stress eating meant eating handfuls of nuts and bags of Five Guys french fries, daily cravings for chocolate and of course sugar. Oh and by the way, I also ordered extra spinach and Kale on my gluten-free pizza and regularly ordered beet salad thinking that would be a better choice.
Before long I couldn’t walk without excruciating pain in my feet- right worse than left and the arthritis pain in my right hip made it hard to stand wearing my 25 lb lead apron in the procedure room. Life was not good. Before realizing that my pain stemmed from an oxalate issue, I tried regular massage therapy, physical therapy, aquatic exercise, cold laser, CBD, and supplements to reduce inflammation and NSAIDS all to little avail.
Then one day I had an epiphany. With every step, I felt like I was walking on ‘shards of glass.’ Limping and discouraged, I consulted Dr. Google. After searching ”what causes you to feel like you are walking on shards of glass”? The answer appeared! Oxalates! I read with great interest all available information about the little-known link between oxalates and pain. This blog will hopefully connect the dots between pain and oxalates making it easier to solve some of your own medical mysteries. I’ll share what I have learned from this painful lesson and what I put into practice to heal myself and hope that this information is helpful to you or any loved one who is hurting.
This topic is important because high oxalates in the body (hyperoxaluria) can be a factor in many chronic conditions; including digestive and urologic issues, autoimmune disorders, and neurological conditions. Oxalates affect mitochondrial function causing fatigue and muscle soreness as well as creating inflammation and unnecessary oxidative stress and free radicals (a very bad thing) — thus potentially influencing every system in the body.
Let’s explore the repercussions of the oxalate cascade in a variety of chronic diseases. The following is an overview of oxalates and is a deep dive into the condition called oxalate crystal disease and the association between oxalates and other potentially related conditions including kidney stones, interstitial cystitis, prostatitis, vulvodynia, autism and atherosclerosis. Basically, there are at least three reasons why people have oxalate issues and some people have all three:
- High oxalate diet — think ‘healthy’ green smoothies, spinach, nuts, etc.
- Candida (yeast) overgrowth in the gut, resulting in high oxalates
- Hereditary hyperoxaluria — kidney stones
Why are oxalates important?
Oxalates present in our body as sharp crystals or crystalline structures with jagged edges that cause pain, irritation, and distress. Oxalates can bind with certain minerals; particularly calcium and magnesium, as well as iron and copper. Calcium oxalates often precipitate in our tendons, fascia, ligaments and joints as well as in arteries and in the urinary tract in the form of kidney stones. Julie Matthews shares this in her blog, Oxalates: Their Influence on Chronic Disease
Where to start your oxalate journey? Food.
Diets high in oxalate could create a wide variety of problems for some people. Modifying a diet to reduce oxalates can make a dramatic difference in lowering the oxalate load. It is important to reduce oxalates in the diet very slowly to avoid oxalate dumping. Some people seem to tolerate high-oxalate diets while others do not. For those with oxalate issues, oxalate-rich foods become a problem if you eat too many. You might be surprised to learn that high oxalate foods are often considered healthy and include foods like spinach, kale, green smoothies, beets, almonds, sweet potatoes, potatoes, chocolate, kiwi etc. You’ll find several different lists of low, medium and high oxalate foods online. Note, that there is some variability in these lists. If you are an Apple user there is a free easy to use App you can download called Oxalator which is a helpful color-coded tool to learn about which foods are high in oxalates.
High Oxalate Foods:
The best way to quickly reduce the negative effects of oxalates is to limit medium and high oxalate foods and to take a combination of 50 mg of activated B6 (P5P) plus calcium citrate and L- Lysine 30 minutes before you eat. This oxalate binding protocol helps to bind the oxalates you eat and prevent them from precipitating in your tissues. For more information on oxalate testing and our oxalate protocol please consult with the medical staff at www.BarrCenter.com.
Cases of oxalate poisoning are all unique. This complicates the diagnosis and is likely one reason this is not a well-understood condition. Additionally, it is possible to develop symptoms even when you do not eat high oxalate foods as this could be a time of oxalate dumping. If you are unsure about your oxalate status we can order a Urine Organics acid test to assess whether you have high oxalic acid levels. This test can also help determine if you have Candida overgrowth which is commonly associated with high oxalates as the candida produce oxalates as a byproduct of metabolism. Once we get the test results back, if appropriate we can get you started on our oxalate and/or candida protocols. Please note that while these tests are a useful tool to point to oxalates as an explanation for symptoms they are not necessarily definitive. Thus if you have symptoms that are otherwise poorly understood and believe that you do not tolerate high oxalate foods please listen to your intuition and take the simple steps to improve your overall health.
Online resources to learn more
Online resources to learn more
Good websites offering information about oxalates include:
- SallyKNorton.com — Sally’s site has a downloadable low oxalate e-cookbook and she has basic information about things to know including oxalate dumping syndrome, which can happen if you withdraw oxalates too quickly
- Trudy Scott
- Susan Owen
- Low Oxalate Diet
- Great Plains Laboratory Oxalate Control brochure
- The Vulvar Pain (VP) Foundation
- Nourishing Hope — Julie Matthews, CNC offers a helpful site with nutrition strategies, recipes, science and practical tips
- Trying Low Oxalates — a Facebook group for support and feedback
Oxalate crystal disease
Oxalate crystal disease
How do we know where oxalates will form in the body? Some in the nutrition world believe oxalates can cause issues where you have a ‘weakness’. Some refer to this as our “Achilles heel” or our unique weak spot. For example, I injured my right hip while rock-climbing 15 years ago, so I suspect this is why my right hip is painful when I eat high oxalate foods. You might experience symptoms in your feet, knees, shoulders, elbows, eyes etc. Because there is no single target organ, oxalate-related issues can be hard to diagnose. A good analogy is that solving the oxalate puzzle is like peeling back the layers of the onion.
The condition “oxalate crystal disease” is often associated with kidney stones. But not everyone with an oxalate issue has kidney stones and most people have normal kidney function. One hint that oxalates could be the root of your pain, is a positive family history of kidney stones.
Oxalate arthropathy is a rare cause of arthritis characterized by deposition of calcium oxalate crystals within synovial fluid. This condition typically occurs in patients with underlying primary or secondary hyperoxaluria. Primary hyperoxaluria constitutes a group of genetic disorders resulting in endogenous overproduction of oxalate, whereas secondary hyperoxaluria results from gastrointestinal disorders associated with fat malabsorption or candida overgrowth resulting in increased absorption of dietary oxalate. In severe cases, oxalate crystals can deposit in the kidney leading to renal failure. Calcific tendonitis and fasciitis are also very common.
Since oxalates are primarily eliminated in the kidney, when the kidneys fail oxalates can accumulate throughout the body — a state termed oxalosis. Affected organs can include bones, joints, tendons, ligaments, fascia, heart, genitourinary system, eyes, and skin. Since patients can present with renal failure and oxalosis before the underlying diagnosis of hyperoxaluria has been made, it is important to consider hyperoxaluria in patients who present with unexplained soft tissue crystal deposition. The best treatment for oxalosis is prevention. If patients present with advanced disease, treatment of oxalate arthritis consists of symptom management and control of the underlying disease process.
Excerpt from: Update on oxalate crystal disease
Calcium oxalates and other symptoms
Calcium oxalates and other symptoms
Although most commonly identified with the formation of calcium oxalate kidney stones (oxalate bound to calcium), when unbound, free oxalate can interfere with cellular functions; affecting health on a broader level. It has been shown that oxalates interfere with cellular function and cellular nutrition resulting in increased oxidative stress, mitochondrial disruption and damage, and nutrient depletions. The impact of this triggers widely varied symptoms including fatigue and inflammatory cascades, joint pain or pain anywhere in the body. Chronic low energy is very common because of a reduction in ATP (energy) in the mitochondria. Oxalates could be a hidden source of headaches, urinary pain, genital irritation, joint, muscle, intestinal or eye pain.
Other common oxalate-caused symptoms can also include mood conditions, anxiety, sleep problems, weakness, atherosclerosis, prostatitis and burning feet.
Calcium oxalate crystals can also be found in the thyroid, and ear, leading to hearing loss under some circumstances.
As Julie Mathews points out, “it’s important to note that oxalates can inhibit the absorption of calcium, magnesium, and other minerals; which actually makes oxalates an “anti-nutrient.” Minerals in food become bound by oxalate – for instance, calcium (thereby forming insoluble calcium oxalate) – and cannot then be absorbed properly by the intestinal tract. This can lead to mineral deficiencies, such as calcium and/or magnesium deficiency and potentially explain osteopenia/osteoporosis. This is why the addition of trace minerals is important in the treatment protocol.
In the gut of a healthy person, oxalates typically bind together with these minerals and then they are eliminated in the stool. While this inhibits the absorption of nutrients, beneficially this ensures they are excreted rather than crossing the gut into the bloodstream and causing cellular distress and damage.”
From Julie Matthews: Oxalates: Their Influence on Chronic Disease
The broad impact of high oxalates
The broad impact of high oxalates
When the gut is unhealthy — endogenous oxalate production
When the gut is unhealthy — endogenous oxalate production
Leaky gut syndrome, the health of the gut microbiome and fat malabsorption can influence whether or not a person has an issue with oxalates. Mineral deficiencies can also cause high oxalates as there are insufficient minerals in the gut to bind the oxalates. A history of antibiotic use, dysbiosis or other conditions that negatively affect the microbiome can contribute. Oxalobacter formigenes, a strain of beneficial bacteria that degrade oxalate can be wiped out by a few courses of antibiotics and impact health for months if not years.
With optimal health, good digestion, and mineral intake, calcium would be available for binding to that oxalate; however, when there is excess fat the calcium binds to the fat, allowing the oxalate to be free to get into the bloodstream and into the cells.
A stool analysis can help you determine if dysbiosis and/or fat malabsorption are at play. Symptoms of fat digestion issues such as floating or greasy stools. Working with digestive enzymes, and supporting gallbladder and bile production can be helpful as well as detoxification support.
Nutritional deficiencies and endogenous oxalates
Nutritional deficiencies and endogenous oxalates
Genetic differences and nutritional deficiencies can impact one’s ability to process oxalates. B vitamin deficiencies, including Vitamin B6 and B1 deficiency, can result in endogenously high oxalates. Vitamin B6 is the most critical B vitamin in energy production and the most common B vitamin deficiency. Thus B6 is a critical part of our oxalate protocol. Additionally, Vitamin A deficiency can cause the body to absorb excess oxalate through the gut resulting in worsening oxalate-related symptoms.
Under certain conditions our body chemistry can convert a substance into an oxalate; Vitamin C and the amino acid glycine (a key component in bone broth) can cause problems. Fructose, xylitol, and other sugar alcohols can also convert to oxalates. Diets too high in meat can also be a problem for some.
Oxidative stress, inflammation and glutathione
Oxidative stress, inflammation and glutathione
There are many pieces to this puzzle. High oxalates can lead to oxidative stress, and subsequently inflammation and injury which can cause oxalate stone formation in the kidney, and damage to any soft tissue or area of the body where they interfere with cellular function.
High oxalates increase free radicals and deplete glutathione thus throwing a monkey wrench in our ability to detoxify environmental toxins. Conversely, antioxidants and free radical scavengers can decrease oxalate stone formation in the kidney, as well as reducing the inflammation caused by oxalate. We have a detox trip protocol at Hang 10 Drips called the Bodhi and this IV therapy protocol can help bring your body back into a healthier state faster through nutrient and glutathione repletion, hydration and free radical reduction.
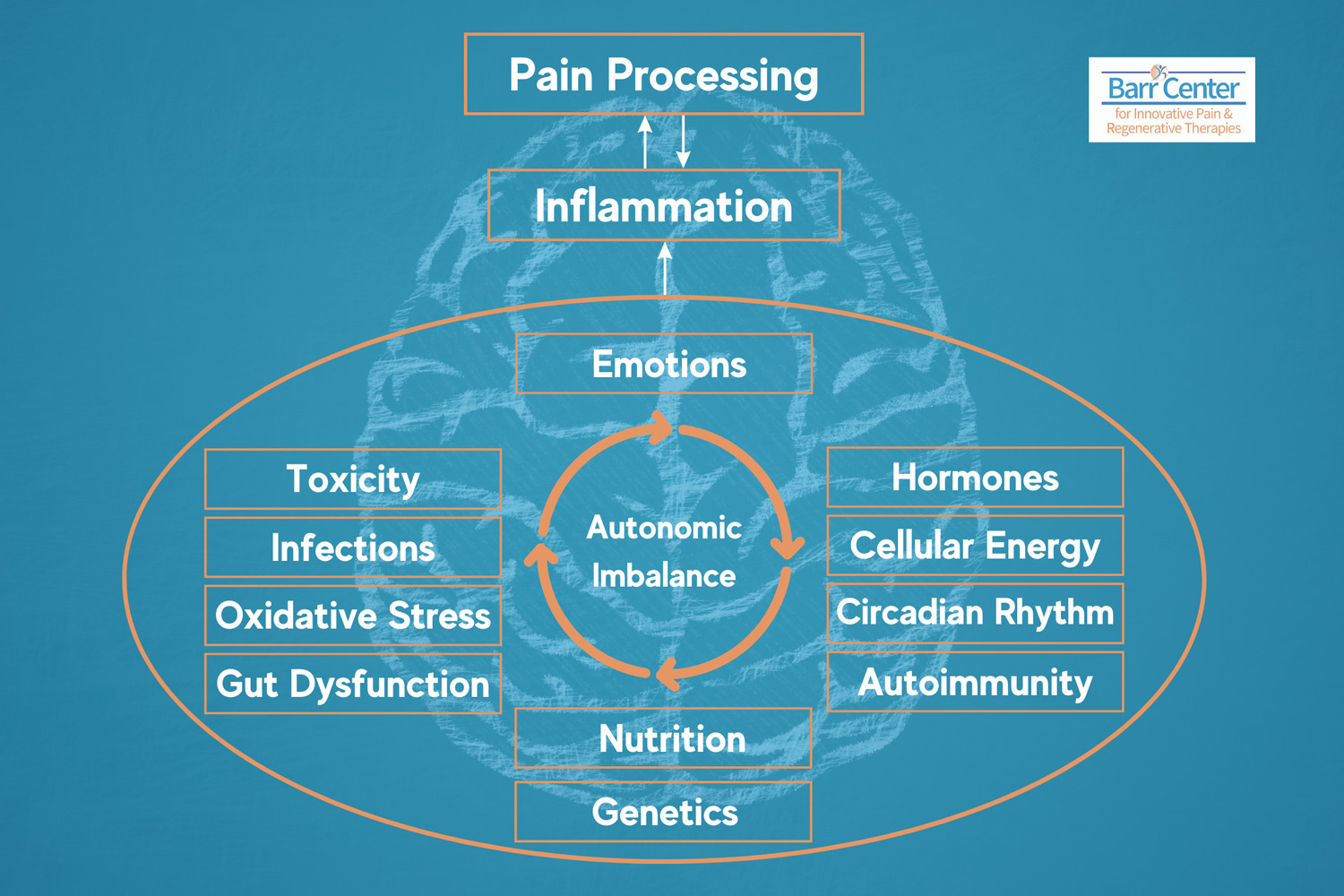
Oxidative stress, inflammation, and low glutathione status are common manifestations in many chronic diseases. Understanding this relationship and the potential sources of chronic inflammation and stress helps us know where to turn to start feeling better. This allows us to address the triggers that can be causing the problems and not just focus on symptoms. Oxalates could be an important factor to consider.
Chronic conditions associated with high oxalate
Chronic conditions associated with high oxalate
If you think that you may have an oxalate-related pain issue and want more information, feel free to reach out to us or schedule a consultation at Barr Center.