Our patients sometimes ask: PRP vs Stem Cells, which is the best solution for my pain situation? Stem cells and platelets work together in your body, complementing one another as they heal injuries and diseases. At the Barr Center, under the direction of Dr. Lisa Barr, we have the option of treating you with several types of regenerative medicine therapies, depending on the nature of your condition and the severity of your pain.
Here’s a rundown of the differences between stem cells and platelets in the form of platelet-rich plasma (PRP) or platelet-rich fibrin matrix (PRFM). Keep in mind that Prolotherapy is one of the original regenerative therapies and it works the very same way in terms of promoting the 3 phases of ‘wound healing’. This important treatment should always be part of the treatment discussion especially in the setting of post-whiplash pain and instability due to ligament laxity.
Different sources — PRP vs Stem Cell
PRP and stem cells come from different sources. PRP is made from platelets extracted from your blood. Stem cells can come from several possible sources-bone marrow and fat derived stem cells are the most common autologous sources and then there are commercially available products from amniotic/umbilical sources which are more costly and do not contain live stem cells.
The idea of autologous sources of growth factors and stem cells implies that we can take your blood and harvest your cells, concentrate the helpful portions and use them to promote healing. Your blood consists of plasma (the liquid part), red blood cells, white blood cells, and platelets. For PRP or PRFM, we take a 30 cc sample of your blood and process it in a centrifuge to separate the platelets from the other components. Then we immediately use a concentrated dose of platelets for your PRP or PRFM injection. This process happens within an hour in our office.
Adult stem cells are being used now in a variety of medical conditions and this new frontier of medicine is really exciting but FDA regulations make widespread availability somewhat limited. When needed for an extra therapeutic boost, stem cells can be harvested from your body fat and/or bone marrow (BMAC or bone marrow aspirate concentrate) and added to the PRP right in our office.
A simple liposuction procedure can remove a small sample of body fat, while a specialized hollow needle is used to withdraw bone marrow from the hip bone. Then the tissue sample is processed to separate the stem cells, which are a type of adult stem cells called mesenchymal stem cells (MSCs) and then mixed with PRP to activate the stem cells. Fat aspirate can be useful when we need to bridge a significant tendon tear as it forms a scaffold for new tissue growth.
PRP/PRFM: The Backbone of Regenerative Medicine
PRP/PRFM is the backbone of our regenerative medicine approach and, only when this doesn’t work, do we add bone marrow (BMAC) or fat derived stem cells. It is important to understand that unlike steroid injections PRP/PRFM and stem cells are both anti-inflammatory and pro-regenerative. This makes it especially useful in the treatment of arthritis joints allowing us to treat a person with arthritis for many years before they would need a joint replacement and allowing us to treat patients with labral and tendon tears often avoiding the need for surgery.
Platelets activate and accelerate the normal healing process. When you’re injured, they travel through your bloodstream to the damaged tissues and release proteins called growth factors and signaling proteins. The current hypothesis is that the major therapeutic benefits of regenerative medicine treatments come from the paracrine action of trophic factors contained in significant concentrations in PRP which signal and guide helpful cells in your blood to the site of the damaged tissue, accumulating them and triggering them to begin the regenerative process. They release many different growth factors and each one triggers cellular activities that are essential for healing.
Growth factors from platelets and stem cells can:
- Trigger new blood vessel growth
- Activate healing activities in the nearby cells
- Recruit stem cells to the injury
- Regulate inflammation
- Protect healthy tissues
- Form the matrix that supports new tissue growth
PRP and PRFM are growth factor-rich autologous treatments derived from a fresh blood draw. Approximately 30 cc’s of your blood is spun down using a special centrifuge, a desired fraction is then extracted as PRP/PRFM. PRFM is activated immediately prior to clinical use with calcium to release desirable growth factors. Different PRP systems isolate and concentrate various white blood cells in differing concentrations. Our Tropocells system for example yields a monocyte rich, neutrophil poor PRP which is desirable in degenerative and arthritic joints. Additionally, because PRP/PRFM requires processing steps which must be performed on freshly drawn whole blood.
For best results, you must be well hydrated and off of Aspirin and NSAIDS for a week prior to and 2 weeks post injection. The avoidance of platelet altering drugs and supplements such as fish oils and CBD/THC during this time is also helpful to optimize the quality of the PRP/PRFM.
The procedure is performed on the same day and takes about one to two hours from start to finish. At the Barr Center, we only perform image guided injections- x-ray guidance is used for spinal and hip joint injections and ultrasound for most other injections as this ensures optimal needle placement for the best results. Note that blind injections are less accurate and can be hit or miss. In general the difference between PRP and PRFM is that PRP is used to treat osteoarthritis and PRFM is used to address tendon issues and arthritis of the smaller joints. The additional step of adding the calcium citrate to the PRP creates PRFM which is much more viscous than PRP suspending the growth factors and stem cells in a place longer, allowing for a more sustained release of the key signaling proteins.
Figure: Diagram of the separation of the parts of blood with the layers separated based on size. The buffy coat is where the platelets are drawn from, then centrifuged again to create PRP
The Cell Science of Regenerative Medicine
Once platelets are activated, they release alpha granules, which contain growth factors that play a role in mitosis, cellular differentiation, and tissue vascularization. Some of these growth factors have significant clinical advantages in promoting cellular activity and tissue remodeling and are considered desirable for numerous clinical therapies. While it has been reported that a variety of different growth factors and cytokines are released from activated platelets, there are a few key chemical mediators that have been reported to play a significant role in healing processes. They include platelet derived growth factor (PDGF), transforming growth factor beta (TGF-β), vascular endothelial growth factor (VEGF), basic fibroblast growth factor (bFGF), and epidermal growth factor (EGF). TGF-β is an immunoregulatory cytokine that contributes to the suppression of the inflammatory response, VEGF is a growth factor that is associated with increasing vascular permeability, angiogenesis, and also has anti-apoptotic functions]. PDGF, bFGF, and EGF are cellular mitogens that promote growth in a wide array of cell types, and serve an important role in the regenerative process associated with PRP.
To review, the clinical successes of PRP/PRFM support the claim that paracrine action is the primary mechanism of healing when it comes to regenerative medicine therapies. The regenerative ‘magic’ comes from the signaling proteins and growth factors that are released by PRP/PRFM and not by the addition of cells that hone in on damaged or degenerate tissue.
There is a significant amount of variability in growth factor profiles from patient to patient, which could potentially translate to a lack of consistency in clinical outcomes and therapeutic. Studies show that the concentrations of certain factors such as EGF, TGF- β, PDGF-AB, PDGF-BB and IGF-1 have been found to decrease as patient age increases (negatively correlated with patient age). Our clinical experience with PRP/PRFM has shown that as long as one’s platelet count is sufficient the outcome is positive regardless of age. This can assess this with a simple blood test. Furthermore, sex differences have been reported in the literature with higher concentrations of these growth factors found in female patients.
We have been performing regenerative medicine injections for nearly 25 years and have witnessed very positive patient outcomes in a variety of conditions with PRP/PRFM with a very low occurrence rate of adverse events, and while there have not been a large number of randomized clinical trials performed for some of the desired applications, such as ligament and tendon repair, the application of PRP for other conditions such as osteoarthritis and lateral epicondylitis has definitively yielded better results than alternatives such as hyaluronic acid and corticosteroids.
Amniotic-Derived Fluid and Stem Cell Therapy
Amnion-derived “stem cell” injections are a misnomer. Please know that there are no live stem cells in any amnion or placenta derived product. These products consist of a fluid that is a conditioned media created during the growth and culture of cells extracted from the amnion, the innermost layer of placenta acquired from live birth placentas that are harvested and sold to companies that process the tissue and package it for sale. This process involves mechanically separating the amnion from the rest of the placenta. It is then washed several times and then the amnion is enzymatically digested to cleave the bonds holding the desired cells from the membrane. These cells are then collected after isolating them from the remainder of the fluid via centrifugation. As the cells grow in culture, they release a similar milieu of growth factors and cytokines that mimic the previous in utero environment. These growth factors and cytokines condition the growth media they inhabit, while adhering to the bottom surface of the culture flask. The conditioned media, also known as amnion-derived fluid, is then irradiated, freeze dried or frozen and packaged and then used as a treatment for a similar range of clinical conditions as PRP.
Amnion-derived fluid also contains a wide range of growth factors, including VEGF, bFGF, EGF, TGF-β, among many others. The mechanism of action for amnion-derived fluid is also believed not to be similar to PRP as it acts by signaling endogenous resident cells to reduce chronic inflammation and promote regrowth of new tissue. Amnion-derived fluid is delivered as a ready-to-use, off-the-shelf product which requires minimal processing time in the clinic. There are currently no FDA regulations controlling the processing of these amniotic products and thus quality concerns are real roadblocks to regular use. Additionally, the cost of these products is considerably higher than autologous injections and in the great majority of patients we have not been able to justify the added cost or risk of infection to the patient.
Stem Cells and Healing Injuries
Stem cells are responsible for regenerating all the different types of tissues needed to keep your body healthy. These cells have the unique ability to self-replicate as many times as needed to create new cells. Then the new cells develop into any number of different tissues.
Adult stem cells thrive throughout your body, waiting until they’re needed to replace old tissues or repair damaged tissues. Though each type of stem cell regenerates several different types of tissues, most target specific functions.
For example, hematopoietic stem cells regenerate the different blood cells, while MSCs rebuild tissues such as muscles, ligaments, tendons, cartilage, tendons, skin, and fat. At the Barr Center, when needed we use both bone marrow and fat derived stem cells.
Bone Marrow Aspirate Concentrate (BMAC) therapy
While similar to Platelet Rich Plasma (PRP) in its ability to harness the body’s ability to heal itself through the aid of growth factors, BMAC also utilizes regenerative cells that are contained within a patient’s own bone marrow. The marrow contains a rich reservoir of “pluripotent” stem cells that, unlike other cells of the body, are “undifferentiated”. This means they are able to replicate themselves into tendon, bone, adipose or cartilage. These cells stimulate your body’s ability to improve circulation, decrease excessive inflammation and regenerate healthy tissue. In general, PRP/PRFM is more appropriate for mild to moderate osteoarthritis and tendon issues. BMAC mixed with PRP is typically reserved for more challenging cases such as moderate to severe osteoarthritis or other conditions when a more potent healing response is required.
The process of obtaining BMAC requires us to access the reservoir of stem cells in your iliac bone using a needle attached to an extraction device that is very similar to ‘tapping a keg of beer’. This is done sterilely under local anesthesia using x-ray guidance in our procedure room. The procedure is not painful and is safe. Approximately 10 cc’s of bone marrow aspirate is obtained and then mixed with your PRP and then injected into the affected tissue/joints. Fat derived stem cells are obtained using a mini-liposuction and the fat cells are then mixed with PRP and injected into the affected tendon or joint.
Exosomes: What Are They?
Stem cells also help you heal by releasing substances called exosomes. Exosomes are extracellular vesicles that contain biochemicals that stimulate a wide range of healing activities. Exosomes are an exciting frontier in regenerative medicine. Future applications of exosomes include IV exosome therapy for a host of autoimmune conditions and chronic infections such as chronic EBV.
Exosomes may stimulate tissue regeneration, boost your immune cells, transport DNA or RNA, or activate the release of growth factors, to name just a few of their possible roles. Exosomes can also be extracted and injected alone or together with stem cells and/or PRP.
Choosing PRP vs Stem Cells
PRP/PRFM and stem cells effectively relieve pain by healing your injury and regulating inflammation. And they’re both good choices for a range of musculoskeletal conditions including arthritis, low back and neck pain, ligament injuries, tendon and labral tears, tendonitis and bursitis. We may use both at the same time or choose one treatment based on each patient’s health care needs. In general, when tendon issues prevail or we are treating small joints of the hands and feet we will recommend PRFM. When arthritis is the key concern we will usually reach for PRP. Stem cells are reserved for more challenging conditions.
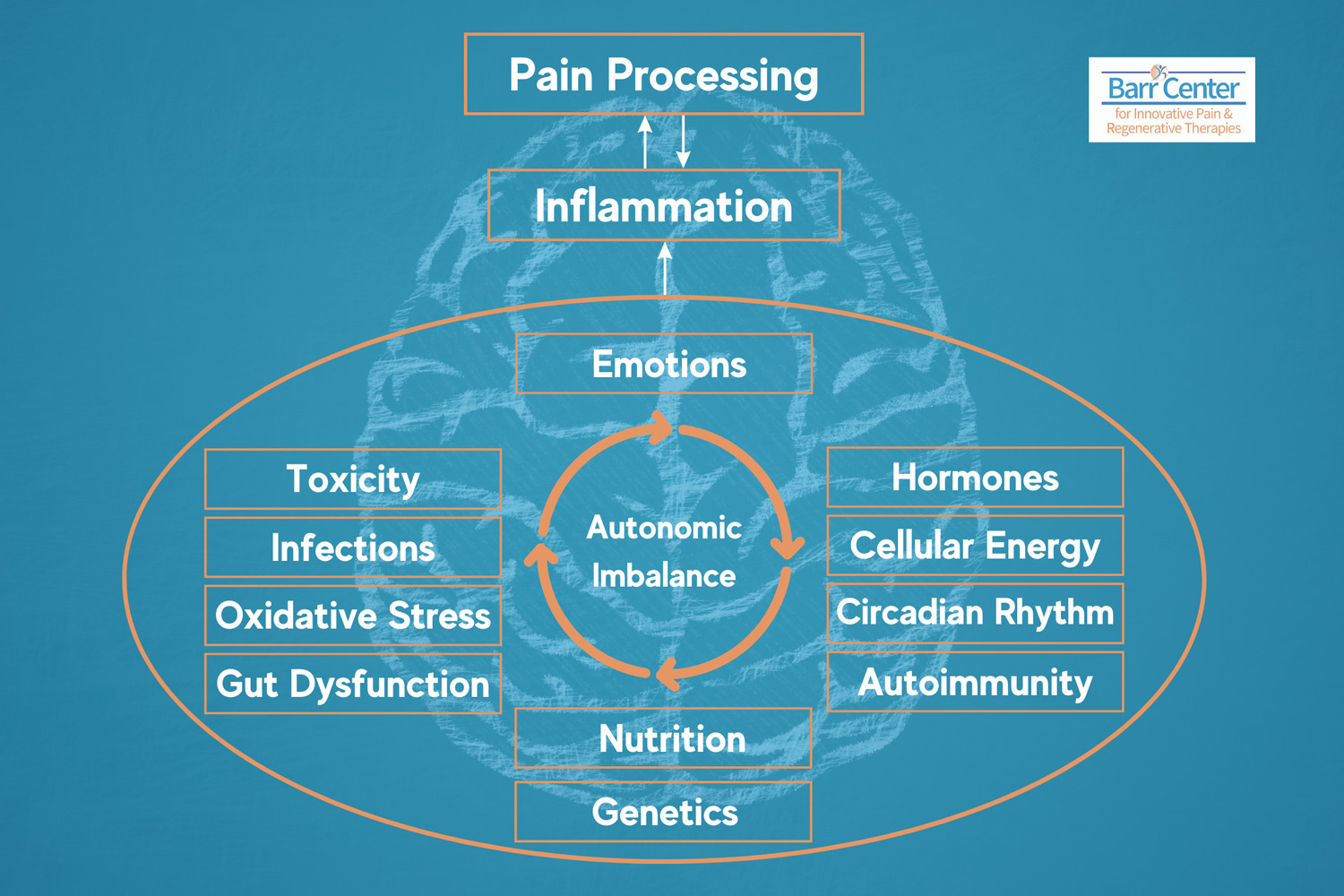
The Barr Center’s Philosophy of Health and Healing
Dr. Barr and her staff are proponents of a functional medicine approach to healing. We believe that given the right conditions the body is capable of healing itself. Sometimes it needs a little help. There are also lifestyle changes you can make to optimize your health and naturally stimulate stem cell production. The following list is a good general recipe to optimize healing and promote natural stem cell production:
- Clean eating such as the Mediterranean or Paleo diet rich in polyphenols
- Intermittent fasting
- Omega 3 fatty acids/EPA
- Eliminating sugar and reducing alcohol consumption
- Optimizing sleep hygiene
- Regular exercise with an emphasis on high intensity interval training (HIIT)
- Minimizing environmental exposure to a variety of toxins as well as reducing EMF exposure
Additionally, we have red and red/violet handheld cold lasers that our patients can rent to treat the injured/affected areas immediately following their regenerative therapies. Cold laser therapy has been shown to facilitate healing by reducing inflammation, stimulating cell growth, and promoting mitochondrial biogenesis.