This Article was featured in www.TidewaterWomen.com on March 1, 2019.
Pain Management: You don’t have to live with pain. Here’s expert guidance on how to live pain-free.
Here’s the sad truth. Many of us have friends, family and neighbors who have been touched in some way by the opioid crisis. Just in the last few months, I know of three families who lost a teenager to an unintentional overdose to prescription opioids.
The CDC reports that 50 million Americans have chronic pain and use opioids to manage pain symptoms. Interestingly, the incidence of pain overall has not increased over the last 20 years, yet the use of prescription pain medication has quadrupled over this same time frame. It seems clear that physicians and the health system as a whole have fallen into a pattern of using opioids as a “quick fix,” failing to consider the nuances of pain and how to best deal with it.
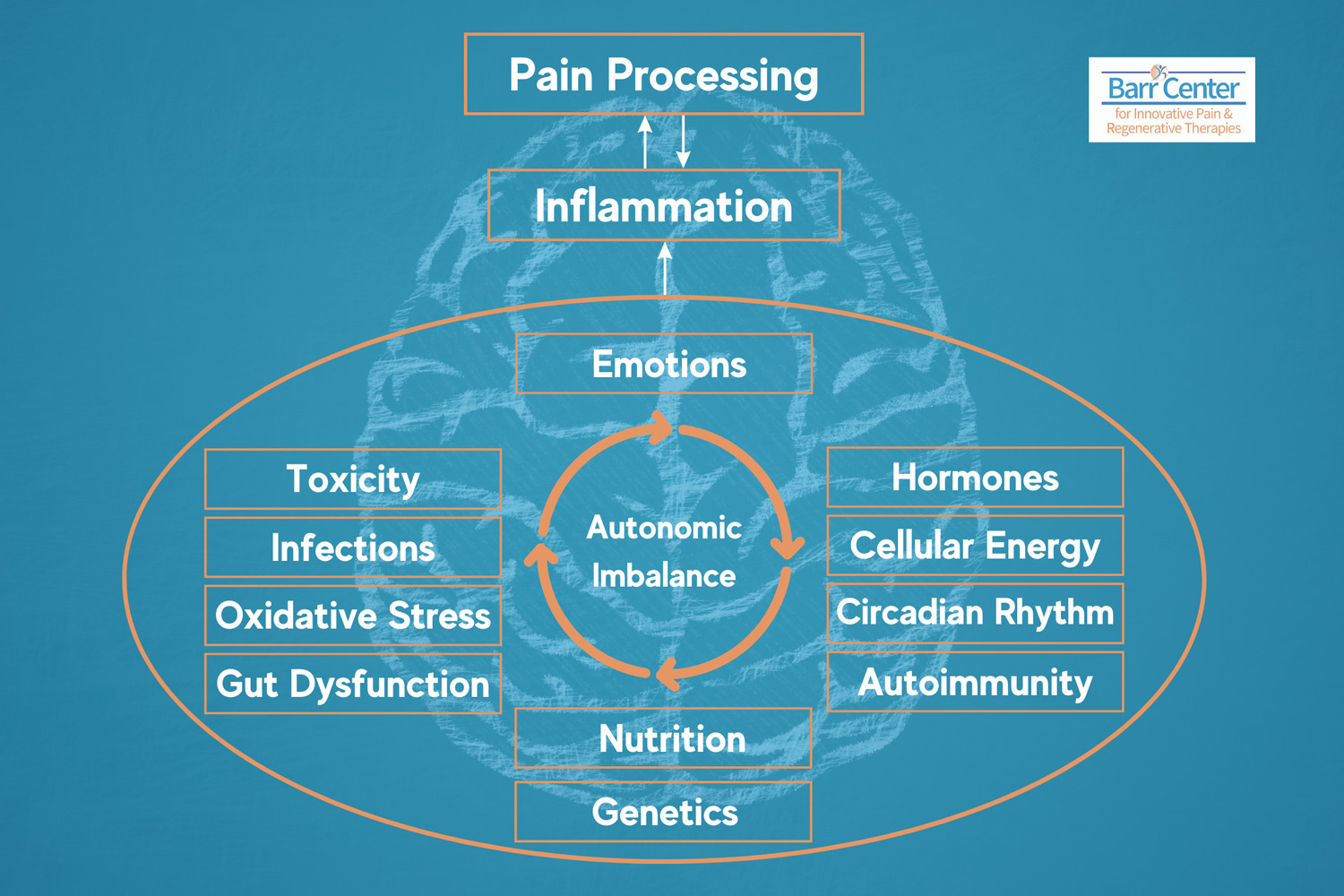
If you explore why quick fixes for pain rarely work, you realize that treating pain effectively requires detective work and a willingness to consider that pain is a sign that something more significant is out of balance in a particular person.
Further, you will learn that not all painful conditions can be diagnosed with an MRI or x-ray. Yes, bones can be broken, discs herniated, and tendons torn, but when pain persists beyond an acceptable healing period of usually 4-6 weeks, then we have to look beyond the tissues for hidden triggers and painful habits that are at the root of the pain.
Habit Patterns Can Lead to Chronic Pain
The Overall Cost of Pain Management Now Exceeds the Cost of Heart Disease, Cancer, and Diabetes

Pain is complex, in part because it is a component of so many medical conditions. It crosses medical specialty boundaries and socioeconomic groups. No one is immune to it. As I explain in my book Outsmart Your Pain! The Essential Guide to Overcoming Pain and Transforming Your Life, pain is the physical expression of the mind-body connection. We feel pain in our body, but its roots can be mental, emotional, and physical.
Pain can also be the result of habit patterns that evolve over time, sometimes in response to a physical injury or overuse. For example, limping after ankle sprain can eventually lead to hip pain and back pain.
For many people pain is rarely just one thing, and the process of teasing out the one core issue at the root of the pain is challenging. Most clinicians do not have the time or training to do the digging necessary to find the core issue causing the pain problem. So they often default to putting pen to paper and prescribing medication to ease symptoms.
As such, pain has now emerged as its own health concern. Because of the multidimensional nature of pain, it is estimated that the overall cost of pain now exceeds the cost of heart disease, cancer, and diabetes.
Another unfortunate truth is that people who lack education and access to good health care and who have limited financial resources have pain that has a much higher impact than those who don’t.
If you know someone in this situation, get them to a pain specialist who does not prescribe opioids because using opioids masks pain and does not address the real problem causing it. You don’t want to risk your life for a pill. Opioids do not fix anything, and unfortunately they trip up many people who have addictive tendencies, causing them to spiral down a dark, dangerous path.
Look for the Underlying Trigger Event for Your Pain
Then Make Effective Lifestyle Changes

The good news is that there is hope for those who hurt. When your back hurts at the end of the day or your tennis elbow keeps you from sleeping at night, seek help from professionals who can help you do the detective work to sort out the cause (trigger) and not the effect (pain).
Look for the underlying triggering event and identify the activity that makes your pain symptoms worse. When you connect these dots, then you can start to make effective changes in your lifestyle that have positive impacts on reducing pain.
In my work I see the most common cause of chronic pain is a sedentary lifestyle. Sitting too much is the number one culprit. Even the American Medical Association agrees. Their new mantra is “Sitting is the new smoking.” Our bodies are designed to move throughout the day, and when they don’t, problems can result.
Additionally, pro-inflammatory diets consisting of processed foods and artificial sweeteners, etc. cause GI issues like IBS and leaky gut that contribute to pain and other health issues. Maladaptive stress responses are also a very common cause of pain. This can manifest as excess muscle tension, poor breathing, headaches, forgetfulness, postural disturbances, and reactive emotional patterns.
There is hope! Studies now show that mindfulness, self-awareness, and self-acceptance practices are effective tools to effectively cope with stress. Even better these techniques are not hard to learn.
Mindfulness Helps You Cope with Pain
Learning How To Get In Touch With Your Body Is An Essential Skill

As part of our treatment approach, we encourage our patients to download a mindfulness app on their smartphones and start simple mindfulness practices, which can make a big difference in coping with painful conditions. Learning how to get in touch with what your body is trying to tell you is an essential skill that can be learned.
When pain gets intense, we often want quick relief, but maybe your pain is there to signal you that something needs to change—a warning light of sorts. Escaping pain with drugs or alcohol isn’t the best answer. Instead pay attention to your body, how you feel, and how stress, your posture, activities, and diet might be impacting your health and causing your pain. Try journaling about how your body feels from day to day and see if you can identify your unique triggers.
One thing for sure is when the mind is calm and the body feels supported, we find ourselves in an ideal state of balance and resilience. Even if you pull a muscle or herniate a disc, when your mind and body are in ideal balance, then pain has little room to roost.
Pain management specialists like myself are physicians trained to assess the complex nature of the pain. We can tease out whether you have a disc issue, arthritis, bursitis, or painful manifestations of excess stress. We can determine quickly if your body is out of alignment or your lifestyle or diet needs some adjusting. We have the hands-on tools and active listening skills to hear your story and quickly decide how to intervene on your behalf to eliminate or reduce pain, so you can move forward with your life.
Lisa Barr, M.D. is a best-selling author and board-certified pain specialist with 30+ years of experience treating pain. She and the staff at the Barr Center for Innovative Pain & Regenerative Therapies, located at 933 First Colonial Road in Virginia Beach, Va. look forward to serving those who have pain and are looking for non-surgical, opioid-free pain solutions. For more information, please visit barrcenter.com.