
Post Laminectomy Syndrome (Post-Surgical Pain or Failed Back Syndrome)
Recurring pain in the back or legs is a fairly common occurrence for patients who have had spinal surgery. This condition is known as Post Laminectomy Syndrome (Failed Back Syndrome). The term “Failed Back” is a misnomer, as it is used to describe a surgery that did not have the desired results from the back or spine surgery, and pain persists.
What are the symptoms?
Symptoms can include dull and aching pain in the back and/or legs as well as stabbing pain in the feet. The pain can be persistent, severe, and debilitating.
What factors contribute to the condition?
- Recurrent disc herniation
- Retained disc fragments
- Incomplete decompression of disc
- Persistent pressure on nerves
- Joint instability or changed joint mobility
- Scar tissue
- Sleep deprivation
- Weakness in muscles that support the spine
- Depression and/or anxiety
How is the Post Laminectomy Syndrome diagnosed?
A variety of state-of-the-art techniques, along with an interdisciplinary approach, have proven effective in diagnosing, managing, or eliminating post-operative pain.
First we conduct a comprehensive examination. Then we may recommend diagnostic studies to help us pinpoint the source of the pain. These can include MRIs, X-rays, nerve conduction studies, and diagnostic spinal injections that are done under fluoroscopy.
How is the Post Laminectomy Syndrome treated?
The syndrome should be treated with an interdisciplinary approach working toward a common goal for the patient. This therapeutic approach could range from non-surgical to surgical intervention.
Therapeutic techniques that have proven effective include:
- Physical therapy
- Modalities
- Manual therapy
- Stabilization education
- Postural education
- Medications
- Antidepressants
- Assessment of opioid protocol
- Antiepileptic drugs
- Injection therapy
- Nerve root blocks
- Epidural injections
- Non-surgical pain management procedures
- Pulsed radiofrequency deactivation of dorsal root ganglion
- Spinal cord stimulation (Dorsal column stimulator)
- Racz procedure (Epidural neuroloysis)
Treatment of Post Laminectomy Syndrome requires a comprehensive evaluation of the causative factors and effects on the patient’s function. Utilizing all of the diagnostic tools that are available and our expertise in providing the care, as well as patient education, we strive to assist our patients in achieving the best possible outcome that will lead to improved function as well as improved quality of life.
What is the Racz Catheter Procedure (Epidural Neurolysis)?
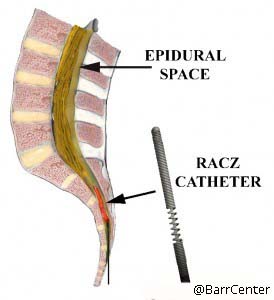 The Racz Catheter Procedure (Epidural Neurolysis) is used to release some of the scar tissue from around entrapped nerves in the epidural space of the spine, so that medications such as cortisone can reach the affected areas. It is used to decrease the pain caused by the scarring. This procedure is named for the physician who pioneered it, Dr. Gabor Racz. Dr. Barr had the good fortune to train directly under Dr. Racz.
The Racz Catheter Procedure (Epidural Neurolysis) is used to release some of the scar tissue from around entrapped nerves in the epidural space of the spine, so that medications such as cortisone can reach the affected areas. It is used to decrease the pain caused by the scarring. This procedure is named for the physician who pioneered it, Dr. Gabor Racz. Dr. Barr had the good fortune to train directly under Dr. Racz.
What causes epidural scarring?
Epidural scarring most often occurs from bleeding into the epidural space following back surgery and the subsequent healing process where epidural fat is replaced with fibrotic tissue. It is a natural occurrence following surgical intervention. Sometimes scarring can also occur when a disc ruptures and its contents leak out.
How long does the procedure take?
The procedure generally takes between 30 and 60 minutes. It can be done once, or in a series of up to three injections in a twelve-month period. A catheter is inserted in the caudal epidural space and steered up to the area of scarring. This is done in our fluoroscopy suites under sterile conditions with IV sedation.
What is actually injected?
The injection consists of the following:
- A mixture of local anesthetic (such as Lidocaine or Bupivacaine)
- Steroid medication (Triamcinolone – Kenalog)
- X-ray contrast so that the scarred space can be clearly visualized
- Concentrated sterile salt solution to soften scar tissue
The procedure involves inserting a needle through skin and deeper tissues. There is some discomfort involved, which will feel like getting a tetanus shot or skin prick. The skin and deeper tissues are numbed with a local anesthetic prior to insertion of the spinal needle and catheter.
Will I receive any sedation for this procedure?
This procedure is done under a combination of local anesthesia and IV sedation, which makes the procedure easy to tolerate. The amount of sedation given will generally depend upon the patient’s tolerance. Communication with the patient during the procedure is important to help assess the proper placement of the catheter.
What should I expect during and after the procedure?
This procedure is done with the patient lying on his or her stomach. The patient is monitored with EKG, blood pressure cuff, and blood oxygen-monitoring devices. The skin is prepped with an antiseptic solution before the procedure is performed under X-ray guidance (fluoroscopy), which is used to assist the placement of the catheter and perform the epidurogram.
After the procedure you will be able to gradually get up and walk into the recovery area. Your legs might feel slightly heavy or numb. You may also notice that your pain may be gone or significantly reduced. This is due to the local anesthetic injected. Although this will last only for a few hours, driving is prohibited following the procedure that day.
 When can I return to work?
When can I return to work?
Unless there are complications, you should be able to return to work the day after the procedure. The most common thing you may feel is a sore back.
How long will the effects of the medication last?
The immediate effect is usually from the local anesthetic that was injected. This effect will usually wear off in a few hours. The cortisone usually starts working in about 3 to 7 days and the effect can last for several days up to a few months.
 Will the Racz procedure (Epidural Neurolysis) help me?
Will the Racz procedure (Epidural Neurolysis) help me?
It is very difficult to predict if the procedure will help you or not. Overall, patients who have recent scarring, such as scarring following recent back surgery, will respond better than those with more long-term scarring. Patients with leg pain and low back pain often report excellent relief of leg pain and some relief of low back pain.
What are the risks and side effects?
Overall, this procedure is safe. However, with any procedure there are risks, side effects, and the possibility of complications. Fortunately, the serious side effects and complications are uncommon. Risks and side effects may include the following:
- Pain/soreness – the most common side effect, and it is temporary
- Urinary difficulty – Occasionally, people report some difficulty urinating for the first several hours post procedure, but this is temporary.
- Other risks associated with the Racz procedure can include:
- Spinal puncture risk/side effects, such as:
- Headaches
- Infection
- Bleeding inside the epidural space with nerve damage
- Worsening of symptoms
- Cortisone injection risks/side effects, such as:
- Weight gain
- Increase in blood sugar (mainly in diabetics)
- Water retention
- Suppression of the body’s own natural production of cortisone
Who should not have this procedure?
You should not have this procedure performed if:
- You are allergic to any of the medications to be injected.
- You are on a blood-thinning medication (e.g., aspirin, Coumadin®, Plavix®).
- You have an active infection.
We generally do not perform more than three injections within a 12-month period. Very frequent injections may increase the likelihood of side effects from the steroid.
Are there any risks with this procedure?
This is considered a very safe procedure. However, as with any procedure, there are risks and possible side effects or complications.
The complications from the selective nerve root blocks and epidural steroid injection include:
- Pain at the injection site – common
- Worsening of symptoms – occasional
- Infection – rare
- Bleeding – rare
- Serious nerve or spinal cord injury – extremely rare
Other side effects are generally related to the steroid medication and may include:
- Fluid retention – uncommon
- Weight gain – uncommon
- Elevated blood pressure – uncommon
Can the Barr Center Help You with Back Pain Relief?
Call us at 757-578-2260 or email us at Info@BarrCenter.com to get started on relieving your back pain.
Learn More
Other pain management conditions we treat are: Neck Pain, Shoulder Pain, Hip Pain and Knee Pain. We often use Regenerative Medicine and sometimes combine Physical Therapy in our treatments.









