Many people consult me about the best way to manage their chronic pain. It’s true; my passion lies in assessing each patient and finding the best solution to resolve their pain–whether it’s a herniated disc, torn tendon, inhibiting scar tissue or a weak muscle. Sometimes, however, the root cause of their pain lies deeper. When this is the case, we have to employ more comprehensive testing to identify why they have persistent pain, inflammation or autoimmunity. This approach to more complex pain resolution is often referred to as Functional Medicine (FM).
FM holds the keys to a deeper understanding of the myriad of potential causes of pain, illness and autoimmunity (as reflected in the diagram above). FM looks at hidden issues, occurring at the cellular and metabolic levels. That throws our bodies out of kilter. Not everyone who has pain needs a FM work up. But when your pain problem cannot be solved easily, it is comforting to know we have the wherewithal to seek deeper answers.
More people are becoming aware of FM as they seek to address the root cause of their medical issues, rather than just taking a pill to manage symptoms. A work up is best done following an FM consult, during which a timeline of symptoms is established and an initial round of tests are ordered. Please note that most FM testing is considered “not covered” under Medicare and most health insurance plans. A follow-up visit is scheduled to review the test results and establish an initial care plan. This can be done in person or virtually, as long as the patient is a resident of Virginia or North Carolina. Keep in mind that the goal of the initial FM work up is to pare down the likely imbalances at the root of symptoms. Depending on the findings, further testing may be needed, as well as coordination of care with other healthcare providers.
To be clear, not everyone with chronic health challenges has pain, and thus FM as a specialty can provide the answer to many confounding symptoms. Because our role at Barr Center for Innovative Pain & Regenerative Therapies is pain management, we can only see patients with pain. For those who need other FM services, we can steer them in that direction.
In my book Outsmart Your Pain the Essential Guide to Overcoming Pain & Transforming Your Life, I also explain how the brain and nervous system play a large role in our experience of pain. People often forget about this when it comes to pain, particularly chronic or recurring pain. To clarify, when we experience acute pain, such as an ankle sprain or torn rotator cuff tendon, our brain interprets painful sensations from the “bottom up,” telling us to immediately attend to an injury. Muscles in the area often go into spasm to protect the area, and our range of motion becomes limited.
On the other hand, chronic pain processing is far more complex, with many top-down and bottom-up influences as outlined above. With the recent advances in neurosciences and new testing around genetics, hormones and gut health, we no longer have to rely on the old paradigm of taking a “pill for every ill.” We can stop and look for the root cause and then address pain with the full expectation that the symptoms will improve with time. We also know how inflammation and other issues can affect the autonomic nervous system, leaving people stuck in a state of “fight or flight .” This is commonly seen with post-traumatic stress disorder (PTSD) and substance abuse disorders.
Pain can be a complex problem to solve.
As outlined in the diagram below, processing pain in the brain has inputs from many components. In fact, the brain plays such a huge role in pain perception that more books are being written about the power of neuroplasticity or the ability of the brain to change under certain influences.
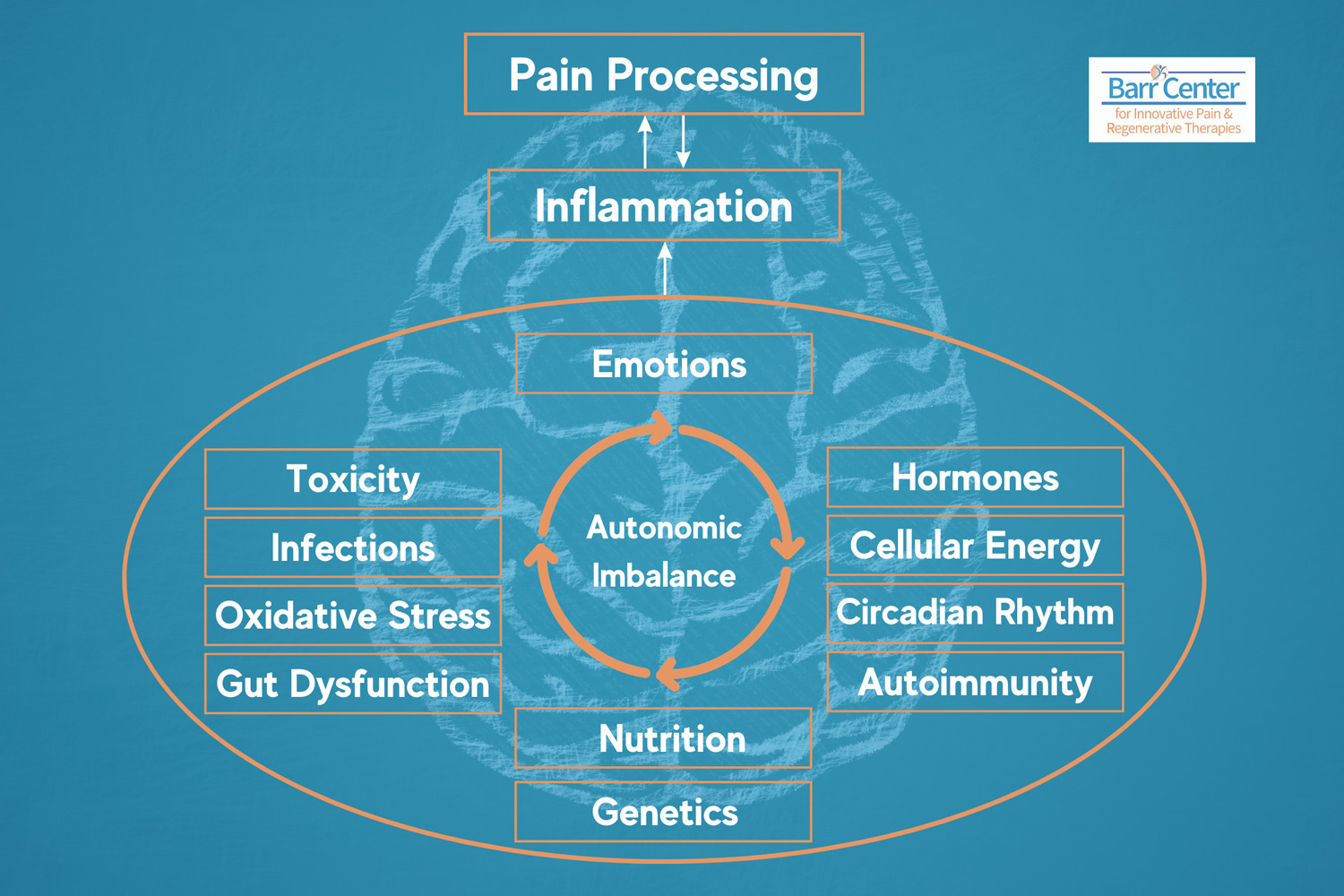
At Barr Center, we are keenly aware of the complex nature of pain. Our mission is always to work a little “pain magic” for our patients, but sometimes there are several variables standing in the way of that magic. Is the “glitch” causing the pain physical, neurological, psychological or physiological? This is the first question we ask. Because the answer is not always clear from the outset, we have the ability to incorporate the more comprehensive FM approach to identify root causes, such as hidden inflammation and infections. This is where FM testing–to include gut health, hormone health, toxicity testing, genetic testing, food sensitivity testing–can be very helpful in giving our patients with chronic pain a leg up on their healing journey.
If you are someone who has not responded to a quick-fix approach to your pain, and know there is more to the equation, call us and come in for a comprehensive FM assessment. We can guide you through this complex process.